Shared Medical Appointments (SMAs)
Shared Medical Appointments (SMAs) are a widely underutilized delivery strategy - in-person or virtually - for effective and efficient care that can be reimbursed by insurers.
In SMAs, also called group medical visits, multiple patients with the same medical condition join a group with a clinician. As a result, providers can spend one to two hours with patients providing both high-yield education as well as patient-specific treatment plans, resulting in a better experience for patients and providers alike. SMAs leverage a “one-to-many” approach to clinical care efficiency that is missing today.
The research is clear: SMAs improve patient health, access to medical care, and provider joy. Importantly, SMAs can also be reimbursed by insurance (although billing practices vary widely; see below), providing a financially sustainable path to incorporating lifestyle medicine into routine clinical care.
Since the 1990s, health systems have slowly been incorporating SMAs into clinical care. Some notable examples of large SMA programs can be found at Massachusetts General Hospital, Cleveland Clinic, Veterans Administration (VA), and Corewell Health. There are countless other clinics and health systems across the country utilizing SMAs, but many face significant - yet often surmountable - barriers to launching and scaling SMAs.
SMA Overview Video
How to Bill for Shared Medical Appointments
There are no national billing guidelines for SMAs. As a result, SMA billing practices vary widely.
This has created a tremendous amount of confusion over the years, resulting in providers being unable to work with their clinics or health systems to launch SMA programming.
However, there are “best practices” from the past 30 years that SMA providers can potentially use to get reimbursed for every patient at every visit.
At the end of the day, it is imperative that you review your SMA billing practices with your Billing Compliance team.
Your Next Step
Before starting your SMAs, your must confirm with your colleagues who oversee billing and compliance that the codes that you plan to use will be approved by your clinic and/or health system and that your note templates comply with established guidelines. It is best to coordinate direct contact from your billing and compliance colleagues to insurance companies to ensure agreement about next steps. For your reference, here is the advice from the American College of Physicians: “ACP recommends that physicians inform each insurer in advance of their intent to begin furnishing group visits and how they plan to bill for them, thus giving the carrier an opportunity to communicate any concerns it may have or request an alternative billing arrangement… Before billing Medicare for group visits a physician should definitely contact the Medical Director of the Medicare carrier in that state to inquire how to bill for services provided to each Medicare beneficiary in a group setting.” Similarly, according to the American Academy of Family Physicians, for “compliance purposes, we recommend that you ask for [payer’s] instructions in writing and keep them on file as you would any other advice from a payer.”
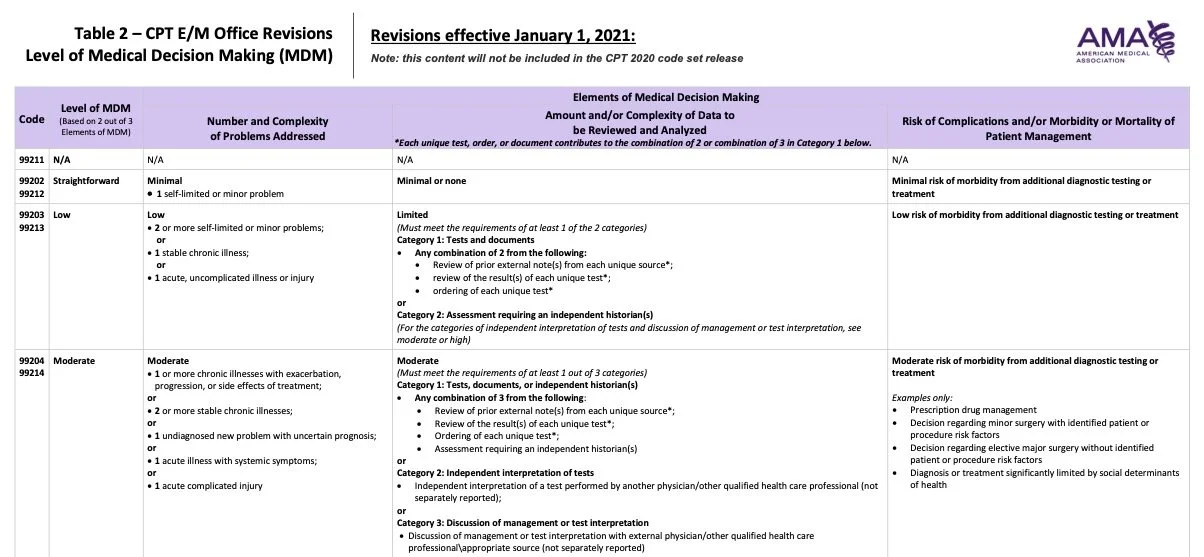
The widely accepted “best practice” for billing SMAs is to treat each individual patient “check-in” that takes place during the SMA as a standard 1-1 follow-up visit. As a result, to meet standard billing requirements for the most commonly used billing codes for 1-1 follow-up visits (i.e., 99212, 99213, and 99214; when appropriate based on Medical Decision Making criteria) is to ensure that:
Every patient receives individualized care from the billing provider during the SMA that is
Documented in the note in the same way as a traditional 1-1 follow-up visit focused on Medical Decision Making criteria
These are based on recommendations from the American Academy of Family Physicians and American College of Physicians as well as the experience of many clinicians and health systems. Said another way, here’s the guidance from the American College of Physicians: “Because group visits are relatively unusual, no nationally accepted standard has yet emerged for billing them, and there is no special code for standard group visits. Acceptable billing thus varies both geographically and among different carriers. In cases where carriers have yet to adopt policies on group visit billing, the practice may be able to gain acceptance of its own proposed methodology - usually billing for each patient individually based on the services documented in the chart just as though the patient had been seen separately.”
Publicly-available resources from Kaiser Permanente and BlueCross BlueShield of North Carolina also supports this approach to documentation and billing.
Individualized Care
Because E/M codes that were developed for 1-on-1 care are typically used in SMAs, it is essential to ensure that you are billing for individualized care within a group context. That is, the decisions regarding data interpretation and/or treatment plans (see table below) should result from an individualized conversation that you have with a patient within the SMA. The outcome of this conversation can then be used in your note as the patient-specific plan for that visit. Although you can comment on any educational or experiential components of your SMA in your note, it is best practice to document patient-specific data interpretation and/or treatment plans to ensure that the E/M code aligns with the individualized care that you are providing to each patient.
Medical Decision Making
Unlike 1-on-1 visits that can be billed based on time, SMAs can only be billed based on Medical Decision Making, which is defined by the American Medical Association (see table below). These recommendations apply to all insurances, including Medicare and Medicaid, which routinely reimburse for SMAs. Although there is no national policy for insurance reimbursement of SMAs, many people point to the published guidance from Blue Cross North Carolina as precedent.
To orient yourself to the table below, which is your key to billing for SMAs, take note in the top left that billing for Medical Decision Making requires “2 out of 3” “Elements” - meaning, you need to satisfy requirements in 2 of the 3 columns on the right. Typically, 99213 codes can be used for SMAs focused on 1) “1 stable chronic illness” with 2) “low risk of morbidity from additional diagnostic testing or treatment,” referring to behavior changes as Lifestyle Medicine-focused treatments. Similarly, 99214 codes can be used for SMAs focused on 1) “2 or more stable chronic illnesses” with 2) either moderate “amount and/or complexity of data to be reviewed and analyzed” (e.g., independent interpretation of tests) or “moderate risk of morbidity from additional additional diagnostic testing or treatment” (e.g., prescription drug management).
Are There SMA Curricula That I Can Use?
Yes!
The SMA materials that Dr. Jacob Mirsky and his team have developed and refined in the MGH Healthy Lifestyle Program are available for licensing so that others don’t waste time reinventing the wheel.
Click here for more information.
For more information
FAQs
-
Absolutely… As long as are meeting standard E/M criteria for Medical Decision Making, and your plan for documenting and billing is approved by your Billing Compliance team.
-
Again, there is no national policy or clear regulation for SMAs. However, the guidance from CMS that is quoted by the oft-cited AAFP website indicates that the answer is “no”:
“No official payment or coding rules have been published by Medicare. However, the question of "the most appropriate CPT code to submit when billing for a documented face-to-face evaluation and management (E/M) service performed in the course of a shared medical appointment, the context of which is educational", was sent to the Centers for Medicare and Medicaid Services (CMS) with a request for an official response. The request further clarified, "In other words, is Medicare payment for CPT code 99213, or other similar evaluation and management codes, dependent upon the service being provided in a private exam room or can these codes be billed if the identical service is provided in front of other patients in the course of a shared medical appointment?" The response from CMS was, "...under existing CPT codes and Medicare rules, a physician could furnish a medically necessary face-to-face E/M visit (CPT code 99213 or similar code depending on level of complexity) to a patient that is observed by other patients. From a payment perspective, there is no prohibition on group members observing while a physician provides a service to another beneficiary." The letter went on to state that any activities of the group (including group counseling activities) should not impact the level of code reported for the individual patient.”
Again, it is imperative that your plan for documenting and billing is approved by your Billing Compliance team.
-
Because our healthcare system is broken! Let’s hope that you’ll be part of the solution.